What is the deadliest neurological disease?
Exploring Multiple Sclerosis
Multiple sclerosis (MS) is a chronic disease that affects the central nervous system, leading to a wide array of symptoms. The immune system mistakenly attacks the protective sheath (myelin) surrounding nerve fibers, causing communication issues between the brain and the rest of the body. Symptoms can vary greatly among individuals and may include fatigue, vision problems, difficulty walking, and cognitive changes. The unpredictability of the disease can significantly impact daily life and overall quality of life.
The course of MS can differ widely from person to person. Some may experience mild symptoms, while others may face severe disability over time. There are several types of MS, including relapsing-remitting MS and progressive MS, which can influence prognosis and treatment approaches. Early diagnosis and a comprehensive treatment plan can help manage symptoms and slow disease progression, making awareness and understanding of this neurological condition all the more essential.
Risk Factors and Prognosis
Multiple sclerosis (MS) has several known risk factors that can contribute to its onset. Genetics play a significant role, as having a family history of MS increases one's likelihood of developing the disease. Geographic location also appears to influence risk, with higher prevalence rates observed in regions farther from the equator. Environmental factors, including vitamin D deficiency and exposure to certain viral infections, have been implicated as potential triggers. Women are more likely than men to develop MS, indicating that hormonal differences may also be a contributing factor.
The prognosis for individuals diagnosed with MS varies widely. While some may experience a singular episode of symptoms, others could endure a progressive form of the disease leading to increasing disability over time. Advances in treatment options have improved the outlook for many patients, allowing for better management of symptoms and slowing disease progression. Early intervention and personalized treatment plans provide hope for a more favorable prognosis, emphasizing the importance of timely diagnosis and ongoing care.
Parkinson's Disease
This progressive neurological disorder primarily affects movement control. Patients often experience tremors, stiffness, and difficulty with balance and coordination. The loss of dopamine-producing neurons in the brain contributes to these symptoms. Over time, individuals may find simple tasks increasingly challenging. Other non-motor symptoms can also emerge, including sleep disturbances, mood disorders, and cognitive changes.
The exact cause of this disease remains largely unknown. Genetic factors may play a role in some cases, yet environmental influences are also under investigation. The progression of the disease varies significantly from person to person. Treatments focus on symptom management and may include medications and lifestyle modifications aimed at improving quality of life. Ongoing research continues to explore potential therapies that could slow or halt disease progression.
Motor Dysfunction and Related Symptoms
Individuals with Parkinson's disease often experience a broad spectrum of motor dysfunction that significantly impairs daily activities. Tremors, rigidity, bradykinesia, and postural instability are hallmark symptoms impacting movement. These abnormalities can lead to difficulties in initiating or executing voluntary movements, which may manifest as a shuffling gait or the inability to make quick turns. Muscle stiffness can exacerbate these challenges, making routine tasks like dressing or eating cumbersome.
In addition to these primary symptoms, patients often report non-motor issues that affect their overall quality of life. Fatigue and sleep disturbances are common, complicating the management of motor symptoms. Emotional changes such as depression and anxiety can also arise, creating a multifaceted challenge for both patients and caregivers. Understanding the intricate relationship between these symptoms is crucial for developing appropriate treatment strategies and interventions.
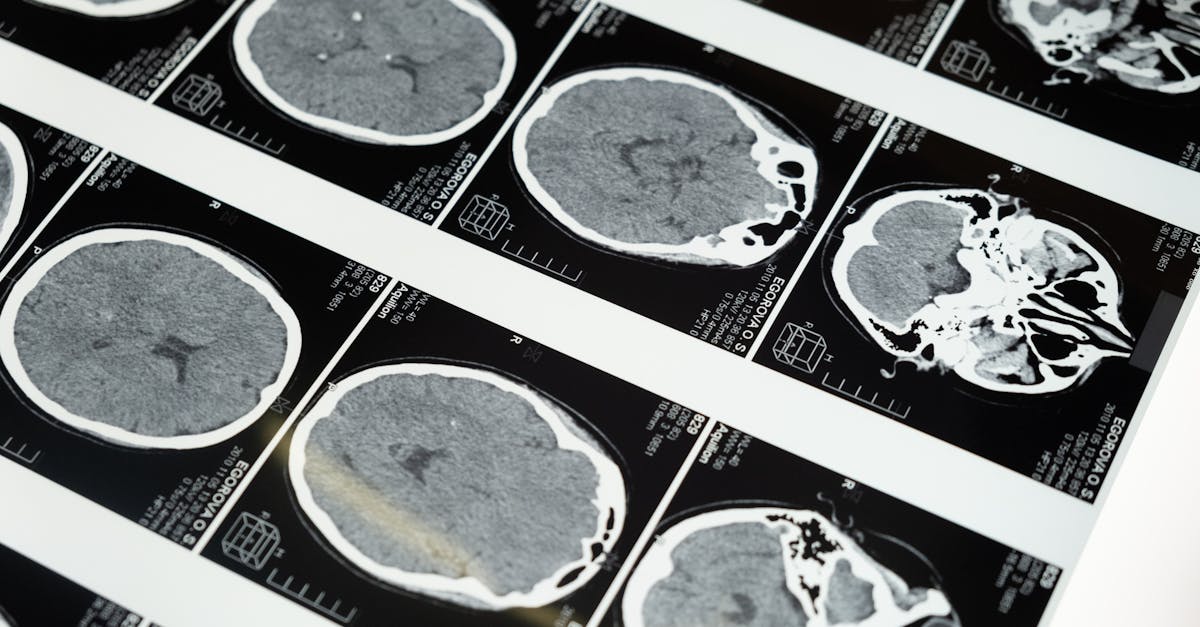
The Severity of Stroke
Stroke represents a significant health crisis, often resulting in severe physical and cognitive impairment. It occurs when blood flow to the brain is interrupted, leading to potential cell death. The severity of a stroke largely depends on its type—ischemic or hemorrhagic—and the area of the brain affected. Prompt medical intervention can mitigate long-term consequences, but many survivors face challenges that alter their daily lives.
Beyond immediate treatment, the aftermath of a stroke can be extensive and complex. Individuals may experience paralysis, speech difficulties, or memory issues that persist for years. Rehabilitation is often necessary to regain lost skills, but recovery can vary widely among individuals. Understanding the unique challenges posed by stroke is crucial for both patients and caregivers in navigating the road to recovery.
Types and Their Consequences
Strokes can be categorized primarily into two types: ischemic and hemorrhagic. Ischemic strokes occur when a blood clot obstructs blood flow to the brain. This type is the most common, accounting for approximately 87% of all stroke cases. Hemorrhagic strokes, on the other hand, arise from a rupture of blood vessels, leading to bleeding in or around the brain. The prognosis for each type varies significantly, with ischemic strokes often linked to conditions like heart disease and diabetes, while hemorrhagic strokes may be associated with high blood pressure and aneurysms.
The consequences of a stroke can be profound and wide-ranging. Survivors may experience various disabilities depending on the area of the brain affected. Common repercussions include difficulties with speech, movement, and cognitive functions. Emotional and psychological impacts also play a critical role in recovery, as many individuals may confront depression and anxiety. Rehabilitation processes can be lengthy and require a multi-disciplinary approach to address the complex aftermath of stroke effectively.
FAQS
What is considered the deadliest neurological disease?
The deadliest neurological disease is often considered to be stroke, as it can lead to significant mortality rates and long-term disabilities.
What are the primary risk factors for developing multiple sclerosis?
The primary risk factors for multiple sclerosis include age, gender (more common in women), family history, certain infections, and geographic location.
How does Parkinson's disease affect motor functions?
Parkinson's disease leads to motor dysfunction through the degeneration of dopamine-producing neurons in the brain, resulting in symptoms such as tremors, stiffness, and difficulty with balance and coordination.
What types of strokes exist, and how do they differ?
There are two main types of strokes: ischemic (caused by a blockage in a blood vessel) and hemorrhagic (caused by bleeding in the brain). Each type has different causes, consequences, and treatments.
Can neurological diseases be prevented?
While not all neurological diseases can be prevented, maintaining a healthy lifestyle, managing risk factors, and seeking early treatment can help reduce the risk of developing certain conditions.
Related Links
What are the five causes of neurological disorders?Can neurological problems be fixed?